Vein Center
 We have operated a comprehensive vein center for over 15 years, led by a highly respected vascular surgeon. Other practices may offer similar treatments as part of their overall services, but vascular treatment is our specialty. Trained in both minimally invasive and surgical treatments, we will offer you specific treatment options that are best for you. As the highest volume vein center in North County San Diego, you can be assured you are in very experienced hands. In addition to Dr. Rayan, we have a licensed full-time vascular ultrasound technician as well as a nurse with 20 years of experience in cosmetic sclerotherapy.
We have operated a comprehensive vein center for over 15 years, led by a highly respected vascular surgeon. Other practices may offer similar treatments as part of their overall services, but vascular treatment is our specialty. Trained in both minimally invasive and surgical treatments, we will offer you specific treatment options that are best for you. As the highest volume vein center in North County San Diego, you can be assured you are in very experienced hands. In addition to Dr. Rayan, we have a licensed full-time vascular ultrasound technician as well as a nurse with 20 years of experience in cosmetic sclerotherapy.
Varicose Veins
What are they?
Varicose veins are abnormally dilated veins in the legs that may cause symptoms. Varicose veins can occur in almost anyone and affect up to 35% of people in the United States. If you have discomfort from your varicose veins, medical insurance usually covers treatment.
Causes and Symptoms
Veins are responsible for bringing blood back to the heart. Gravity can play a big part in working against the venous return in the legs. When you sit or stand, blood tends to pool in the legs. If the valves in the leg veins aren’t functioning properly, the increased pressure in the veins over time can cause varicose veins. People can get varicose veins from advanced age, genetics, pregnancy, or being overweight. Some common symptoms include:
- Aching/Throbbing
- Itching/Burning
- Swelling
- Skin Discoloration
- Leg Fatigue or Tiredness
- Rarely, superficial blood clots or bleeding
Treatments
EVLA (Endovenous Laser Ablation)
Endovenous Laser Ablation or EVLA is a minimally invasive option for saphenous vein reflux (leaky valves). EVLA replaced vein stripping as the procedure of choice to treat venous insufficiency about 20 years ago. The procedure involves using laser energy to “close” as much of the saphenous vein as possible. Because thermal energy is being used, much of the procedure time involves injecting a dilute local anesthetic to numb the area around the vein.
The procedure itself usually takes about 15 minutes. Prep time before and after takes 15 minutes each. Anticipate at least 45 minutes in the office. You will need compression stockings after the procedure for 1 week. The discomfort with the procedure is analogous to a tooth cleaning (1 or 2 out of 10 on a pain scale). You will be awake and comfortable during the procedure. Valium can be prescribed as needed.
Venaseal (Chemical Endovenous Ablation)
This is a relatively newer technique that is covered by some insurance plans. It involves injecting a chemical adhesive into the vein, thereby closing it. Since there is no thermal energy, pain during and after the procedure tends to be rare. Also, compression is not necessary after the procedure. Procedure time is also around 15 minutes. This has become an increasingly popular method to treat venous insufficiency and is an excellent choice for elderly or overweight patients. Click here for additional information and illustrations.
Phlebectomy (Vein Removal)
Phlebectomy literally means “vein removal”. Phlebectomy is a minimally invasive procedure done under general or regional anesthesia to remove large varicose veins using micro-incisions. The procedure typically takes 30-90 minutes and is done as an outpatient. The micro-incisions are each about 3 mm long. Each is closed with a single suture that is removed a week later. Complications tend to be rare. Expect to spend half a day away from home and take a few days off to recover.
Sclerotherapy (Vein Injections)
Sclerotherapy is a popular method for eliminating varicose veins and superficial telangiectasias also known as “spider veins.” Sclerotherapy involves a solution, called a sclerosing agent, which is injected into the veins. We use polidocanol, an injectable solution approved by the FDA to sclerose superficial veins. It is a minimally invasive, highly effective way of decreasing the symptoms associated with venous disease and improving cosmesis. Sclerotherapy is a proven procedure and has been in use since the 1930’s.
The number of treatments needed to clear or improve the condition differs from patient to patient, depending on the extent and size of the veins to be treated. Larger or more numerous veins may require more treatments. Although you will need to wear stockings for a week, you will not need any downtime.
Varithena (Distal Endovenous Chemical Ablation)
Varithena is a special formulation of the chemical used for sclerotherapy, polidocanol. It is designed specifically for larger veins like the saphenous veins- ideally the lower part of a vein that has already been treated. A niche product, Varithena can be a powerful adjunct to laser or Venaseal in treating the entire great saphenous vein if necessary. Click here for additional information and illustrations.
Stroke Vulnerability
What is it?
A stroke is when the blood supply to a part of your brain is suddenly interrupted and part of the brain dies.
Ischemic Stroke: approximately 75% of all strokes, can occur when blood supply to your brain is blocked.
Hemorrhagic Stroke: can occur when there is bleeding in your brain.
Transient Ischemic Attack (TIA) or mini-stroke: a condition similar to stroke, but the symptoms only last seconds or a few minutes and completely resolve within 24 hours. Can be a warning sign of a future stroke, and medical attention should be sought as soon as possible.
Causes and Symptoms
Ischemic stroke and Transient Ischemic Attack (TIA), where the blood supply to a part of your brain is interrupted, is most commonly related to high blood pressure (hypertension), which can damage the small blood vessels in your brain. Abnormal heart rhythms, such as atrial fibrillation, which can cause small blood clots to travel from your heart can also be a cause. Hardening of the arteries (atherosclerosis), a buildup of plaque in the carotid arteries that bring blood to your brain is something we can help with. Plaque can build up over time in arteries as you get older due to long-term effects of illnesses like high blood pressure, high cholesterol levels and diabetes. Pieces of this plaque can break off and travel to your brain which can cause a stroke.
Some symptoms occur suddenly and include:
- Numbness
- Confusion
- Trouble Speaking
- Trouble Walking
- Severe Headache
- Trouble seeing with one or both eyes
Hemorrhagic Stroke is bleeding within your brain and is typically caused by:
- Head or brain injury
- Certain types of congenital brain aneurysms
- Very high blood pressure and bleeding from arteries
Treatments
TCAR (Transcarotid Artery Revascularization)
TCAR is stenting the carotid artery using a device that briefly reverses the direction of blood flow. With blood flowing away from the brain while the physician operates, the patient’s risk of stroke during the procedure is lower. The procedure is performed by performing a small incision above the clavicle and placing a tube in the carotid artery. The system will temporarily redirect blood flow of plaque away from the brain and then the filtered blood is returned to an area below the waist. Stenting the artery opens the artery and assists in preventing strokes.
CEA (Carotid Endarterectomy)
Carotid endarterectomy is a surgical procedure to open or clean the carotid artery with the goal of stroke prevention. It is an extremely durable procedure. Carotid endarterectomy is performed in an operating room under general anesthesia. Typically, only an overnight hospital stay is required. The plaque is removed through a small oblique incision in the neck. After removing the plaque from the artery your vascular surgeon repairs the artery by sewing a woven patch onto the artery to prevent re-narrowing. it is the most common surgery utilized for stroke prevention in the US.
Peripheral Arterial Disease
What is it?
PAD is a chronic disease in which plaque builds up in the arteries to the legs. This buildup typically occurs gradually. If allowed to progress, blood flow in that artery can become limited or blocked all together. PAD is relatively common, affecting more than 10 million people in the U.S. It is more common in people who are 65 or older, usually in smokers and diabetics.
Causes and Symptoms
The causes of PAD include smoking, high cholesterol or high triglycerides, high blood pressure, diabetes, kidney failure, and obesity. Genetic factors also play a role. Many patients may not experience any symptoms. Some noticeable symptoms can include:
- Fatigue or cramping of muscles while walking
- Pain in toes or feet while resting
- Non-healing wound on toes or feet
Treatments
PAD is usually treated by aggressively managing the risk factors with lifestyle changes and medication. This includes quitting smoking, controlling blood pressure and cholesterol, controlling diabetes, and losing weight. In addition, an exercise program, if followed faithfully, can significantly improve the symptoms of PAD in many cases.
Symptomatic PAD can be treated with techniques such as balloon angioplasty or stent placement. These procedures can usually be performed in the office setting in about an hour. Dr. Rayan has performed over 3000 of these procedures with excellent results.
For patients with extensive PAD where minimally invasive techniques are not an option, surgical bypass may be necessary.
Deep Vein Thrombosis (DVT)
What is it?
Occurs when your blood thickens in a clump that becomes solid, forming a clot. Most deep vein clots occur in the lower leg or thigh. If a superficial vein is involved, the condition is called thrombophlebitis. The danger of deep vein thrombosis is that the clot can break loose without therapy and cause a pulmonary embolism.
Causes and Symptoms
DVT is often associated with acute inflammation. DVT can occur after a major operation, after trauma or during a flight. Sometimes they can be related to an underlying cancer. Not infrequently, they can simply be unprovoked. Symptoms include:
- Swelling in one leg
- Pain or tenderness in one leg
- Warmth or discoloration in one leg
Treatments
Anticoagulation
The mainstay of therapy is anti-coagulation. Typically, 3 to 6 months of a medication such as Eliquis, Xarelto or Pradaxa are necessary to stabilize the clot.
Thrombectomy
Venous thrombectomy has evolved into the primary treatment for extensive or very symptomatic DVTs. This outpatient hospital procedure involves suctioning the clot out of the leg through a large IV placed behind the knee or in the groin. Recovery is rapid and results are excellent. This procedure can only be performed when the clot is newly diagnosed.
Stenting
Sometimes, DVTs can be due to compression or narrowing of the underlying vein. Using intravascular ultrasound technology, we can identify these problem areas and place a stent to prevent future blood clots.
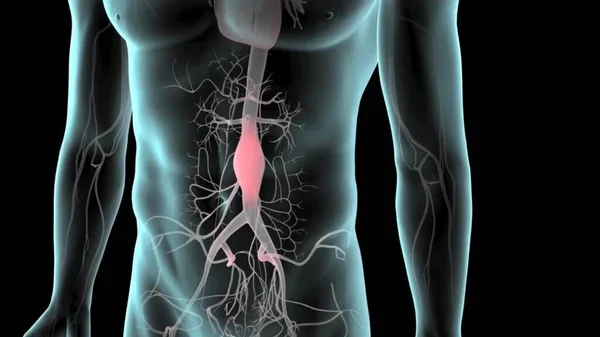
Aneurysms
What is it?
An aneurysm is a bulge or ballooning in a blood vessel that occurs in the wall of a major blood vessel. The abdominal aorta carries blood from your heart to your body and is the blood vessel most frequently affected. If allowed to get too large, an aneurysm can leak or rupture, causing catastrophic internal bleeding. The goal of aneurysm therapy is to treat it before it becomes symptomatic or ruptures. Other sites for aneurysms include the thoracic aorta, the iliac arteries and branch vessels off the aorta.
Causes and Symptoms
Risk factors can contribute the presence of an aortic aneurysm include:
- Older age
- Cigarette smoking
- Family history
Screening
Medicare covers a free screening ultrasound for male smokers or females with family history.
Treatments
Endovascular Aortic Aneurysm Repair (EVAR)
The most common treatment of abdominal aortic aneurysms (AAA) is EVAR. EVAR is a novel method of fixing AAA using stents introduced through both groins to exclude the aneurysm from the rest of the circulation. Typically this is done in around 1-2 hours with a general anesthetic. Multiple stent components are introduced percutaneously to prevent the AAA from rupturing in the future. The procedure is relatively painless and associated with an overnight hospital stay. Results are excellent but long term followup is required.
Open Surgical Repair
The traditional operation involves cutting open your abdomen to replace the aneurysm with an artificial piece of artery (a graft). This is a major operation and carries some risk. However, it is successful in most cases and the long term outlook is good. The graft usually works well for the rest of your life.
Dialysis Access
What is it?
Hemodialysis is a treatment that removes wastes and extra fluid from your blood when your kidneys have failed. Before hemodialysis can be done, a connection must be made to the blood inside your blood vessels. Your hemodialysis access, or vascular access, is a way to reach your blood for hemodialysis. The access allows your blood to travel through soft tubes to the dialysis machine where it is cleaned as it passes through a special filter called a dialyzer.
Your doctor will help determine when you should start hemodialysis based on several factors, including your:
- Overall health
- Kidney function
- Signs and symptoms
- Quality of life
- Personal preferences
Treatments
Hemodialysis Access
Vascular surgeons specialize in creating long-term dialysis access called an arteriovenous fistula. A fistula is a direct connection between an artery to a vein in the arm. This connection makes the vein grow large and strong. The larger vein provides easy, reliable access for hemodialysis nurses. Without this kind of access, regular hemodialysis sessions would not be possible. Untreated veins cannot withstand repeated needle insertions, because they would collapse the way a straw collapses under strong suction. If the arm veins are too small for a fistula, an indirect connection can be performed called an AV graft.
World-Class Vascular Treatment


Conveniently located in Encinitas, our office is ready to give you the personalized treatment you deserve. Contact us to make your appointment now and become one of the hundreds of patients whose lives have been changed by our world-class care.